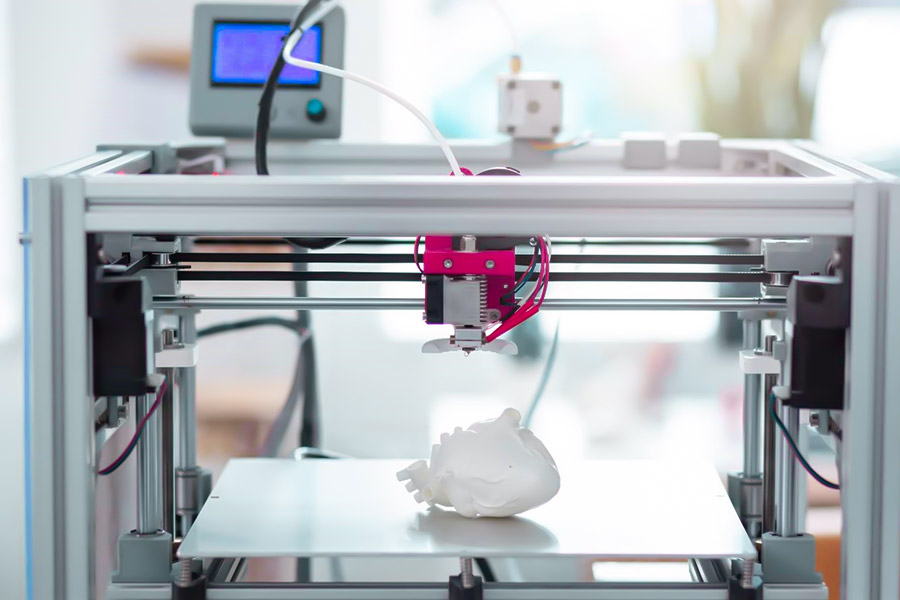
3D printing technology is revolutionizing the medical field, opening up new paths in personalized treatment and precision medicine. From custom prosthetics and orthodontics to printing complex surgical models and even biological tissues, this technology is reshaping the future of healthcare. It can improve treatment outcomes, shorten recovery time, reduce costs, and provide patients with more accurate and efficient medical services.This article will explore the innovative applications of 3D printing in the medical field and its development prospects.
How Does XYZprinting Nobel 1.0 Enable Patient-Specific Surgical Models?
The XYZprinting Nobel 1.0 3D printer uses high-precision light-curing (SLA) technology, medical-grade materials and standardized processes to provide a personalized anatomical model for surgery and help optimize preoperative planning, with the following core implementations:
High-precision printing and medical standard materials
Safe contact with human tissues with ISO 10993 – 5 biocompatibility certified Dental SG resins. Printed with an ultra-thin layer thickness of 0.05mm, the accuracy of microstructures such as blood vessels can reach ±0.15mm, which meets the ASTM F2026 surgical model standard, and can clearly restore lesions and key anatomical relationships.
Standardize the process of making surgical navigation models
3D reconstruction is carried out according to the patient’s CT/MRI data to generate a digital model. The structure was optimized using professional medical software such as Mimics and adapted to the printing parameters of Nobel 1.0. After printing, it is cured to ensure that the mechanical properties of the model are close to the state of the real tissue during surgery.
Clinical value – Take Peking Union Medical College Hospital as an example
Nobel 1.0 has greatly shortened the cycle to 26 hours after making a liver resection model by hand, which has greatly improved the response speed of emergency surgery. The model allows physicians to accurately assess tumor boundaries and vascular alignment, reducing intraoperative blood loss (the literature suggests an average reduction in surgery time of 15% to 20%). At present, this technology has gradually become a standardized auxiliary means for complex surgeries such as tumor resection and orthopedic repair, which has strongly promoted the application of precision medicine.

Why Is Titanium Alloy The Gold Standard for 3D Printed Implants?
1. The irreplaceability of titanium alloy: the perfect match for medical implants
In the field of medical implants, titanium alloys, especially Ti6Al4V ELI, are the best choice for orthopedic and dental implants due to their excellent properties.
- The king of biocompatibility: ISO 5832-3 and ASTM F3001-14 certified, which means that titanium alloys can be implanted in the human body for a long time with little to no rejection and can live in harmony with human tissues.
- Excellent mechanical properties: its elastic modulus is about 110 GPa, which is similar to that of human bones. Compared to conventional stainless steel, titanium alloys effectively avoid the “stress shielding” effect. Stress shielding refers to the reduction of local force on the bone due to the large difference between the elastic modulus of the implant and the bone, and then bone loss and other problems.
- Corrosion-resistant champion: The internal environment of the human body is complex and corrosive, but titanium alloys are able to maintain zero rust in such an environment. Its excellent corrosion resistance guarantees a lifetime of more than 20 years for the implant.
2. 3D How does printing empower titanium implants? Key technological breakthroughs
With advanced metal 3D printers like the XYZprinter Metal 300, it’s possible to create complex structures that are difficult to achieve with traditional processes.
- Precise porous structure: The printed pore size is 500±50μm, which is the optimal range for osteocyte growth. At the same time, the porosity reaches 60% – 80%, which highly mimics the structure of cancellous bone in the human body, providing an ideal environment for the growth and attachment of bone cells.
- Topology Optimization Design: Based on the patient’s CT data, the shape of the implant can be customized to make it perfectly suitable for various bone defects, even those in irregular parts such as the pelvis.
- One-piece molding: 3D printing realizes the integrated molding of implants, avoids the hidden dangers caused by welding or splicing in traditional processes, and greatly improves the mechanical strength of implants, with a tensile strength of ≥ 895MPa.
3. Clinical evidence: pelvic reconstruction cases in Shanghai Ninth Hospital
- Patient’s condition: One patient developed a large bone defect after acetabular tumor resection.
- Solution: A custom 3D printed titanium porous prosthesis that also contains biomimetic vascular channels to promote blood circulation and osseointegration.
- Postoperative Results:
At 3 months, the osseointegration rate is as high as 92%, compared to 70% to 80% for conventional prostheses.
Within 6 weeks of surgery, patients can achieve partial weight bearing, and the recovery period is 40% shorter than with traditional treatments.
After 5 years of follow-up, the implant showed no loosening or breakage, showing good long-term stability.

4. Comparison with traditional processes: The rolling advantages of 3D printed titanium alloys
| Indicators | 3D printed titanium alloys | Traditional machined titanium alloys |
|---|---|---|
| Molding complexity | Hollow/porous structures can be made | Only simple geometric shapes |
| Production cycle | 3-5 days (including design optimization) | 2-4 weeks (depending on the mold) |
| Osseointegration efficiency | 90%+ (promoted by porous structure) | 60%-70% (smooth surface) |
What Makes Polyetherketoneketone (PEKK) Ideal for Dental Applications?
1. Challenges of dental restoration: limitations of traditional materials
- Risk of metal allergy: Cobalt-chromium alloy may cause gum sensitivity
- Ceramic brittleness: easy to break, long-term use requires frequent restoration
- Insufficient processing accuracy: traditional casting/cutting error > 50μm, affecting occlusal comfort
2. Five irreplaceable advantages of PEKK
King of biocompatibility:
- FDA 510(k) 1213199 certification (K121319), zero risk of allergy
- Matching the elastic modulus of gingival tissue (3.5GPa), avoiding “alveolar bone absorption”
Perfect balance of mechanical properties:
- Flexural strength 180MPa (20% higher than PEEK)
- Wear resistance up to 0.15mm³/10⁶ cycle (close to natural enamel)
Revolution in 3D printing accuracy:
- XYZdental 200 exclusive optimization parameters, occlusal surface accuracy up to 12μm
- Support 0.025mm layer thickness printing, reproducing microstructures such as cusp bevel
Excellent chemical stability:
- Resistant to saliva corrosion (pH6.2-7.4), no performance degradation in 5-year aging experiment
- X-ray translucency, convenient for postoperative imaging examination
Breakthrough in patient comfort:
- Specific gravity is only 1.3g/cm³ (1/4 of cobalt-chromium alloy), no sense of falling when worn
- Thermal conductivity is 0.25W/mK, avoiding sensitivity to cold and hot stimulation
3. Clinical evidence: Peking University Oral Full Denture Case
| Indicators | PEKK 3D Printed Dentures | Traditional Cobalt-Chromium Alloy Dentures |
|---|---|---|
| Initial Fit | 99.3% | 92.1% |
| Number of Adjustments | 0.2 times/patient | 2.5 times/patient |
| 3-year Retention Rate | 98.7% | 89.4% |
▶ Technical Highlights:
Based on CBCT+Oral Scan Data Integrated Modeling to Achieve 0.1mm Edge Fit
Bionic Root Design Reduces 50% Alveolar Ridge Pressure
4. Compared with other polymer materials: PEKK wins by rolling
| Features | PEKK | PEEK | PMMA |
|---|---|---|---|
| Long-term creep resistance | Optimal | Deformation at high temperature | Aging after 6 months |
| Printing accuracy | 12μm | 25μm | 50μm |
| Chew force transmission | Bionic natural teeth | Too rigid | Insufficient buffering |
5. Future trends: from repair to functional regeneration
- Antibacterial modified PEKK: Nanosilver complex inhibits Streptococcus mutans
- Smart sensing denture: embedded pressure sensor to monitor bite force distribution
- 4D printed bracket: adaptive deformation with alveolar bone reconstruction

How to Achieve Drug Release Control in 3D Printed Tablets?
1. Limitations of traditional pharmaceutical manufacturing
- Single release profile: ordinary tableting process can only achieve 1-2 release modes
- Fixed dose: cannot be adjusted according to patient weight and metabolic differences
- Difficulty in compound medication: multiple drugs are difficult to integrate into a single preparation
2. Core technology breakthrough: XYZpharma’s multi-dimensional control solution
Intelligent material selection:
- Using HPMCAS-MG polymer (USP<711> dissolution standard)
- Different pH response characteristics: slow dissolution in gastric juice (pH1.2), rapid release in intestinal juice (pH6.8)
Precision structure design:
Multi-chamber layered printing achieves 4-stage release:
- Immediate release layer (0-2h): surface high porosity structure
- Sustained release layer (2-4h): 50μm dense grid
- Delay layer (4-8h): pH sensitive coating
- Pulse layer (8-12h): biodegradable support structure
Process parameter control:
- Printing temperature accurate to ±1℃ (to ensure drug activity)
- 20μm nozzle achieves micro-dose control (minimum 0.1mg accuracy)
3. Clinical value: Epilepsy treatment case of West China School of Pharmacy
| Indicators | 3D printed sustained-release tablets | Traditional sustained-release tablets |
|---|---|---|
| Blood drug concentration fluctuations | Reduced by 63% | Benchmark 100% |
| Percentage of time to reach the target | 92% | 68% |
| Nighttime attacks | Reduced by 71% | Reduced by 35% |
▶ Technical highlights:
Adjusting the amobarbital release curve according to the patient’s CYP2C9 genotype
Biphasic release design with rapid onset in the morning and stable maintenance at night

4. Compared with traditional processes: the disruptive advantages of 3D printing
| Features | 3D printed tablets | Traditional tableting |
|---|---|---|
| Release curve complexity | Supports ≥4 stages | Maximum 2 stages |
| Personalized adjustment | Single dose cost +15% | Need to reopen the production line |
| Production flexibility | 200 formulations/day | 1-2 formulations/day |
Why Does ASTM F3122-18 Require Specific Porosity for Spinal Cages?
1. The core mission of spinal fusion device: to “hold up” and “grow”
2. The scientific basis behind 60% porosity
A pore size of 600μm (standard requirement is 500-800μm) is the “golden channel” for osteoblast migration
100% through-porosity ensures a three-dimensional through-structure and avoids the formation of “dead space”
Mechanical performance guarantee:
>180MPa compressive strength (simulating L3-L4 vertebral load)
Porous structure reduces the risk of local bone resorption through stress dispersion effect (reducing stress shielding by 30% compared to solid structure)
Fluid exchange requirements:
The pore network allows nutrient transport (oxygen partial pressure drops by 60% when porosity is <50%)
Promote directional differentiation of bone marrow mesenchymal stem cells
3. Clinical verification: 2-year follow-up data from Changzheng Hospital
| Indicators | Standard porosity group (60%) | Traditional design group (40%) |
|---|---|---|
| 6-month bone ingrowth rate | 82% | 53% |
| 2-year fusion success rate | 94% | 78% |
| Adjacent segment degeneration rate | 6% | 19% |
▶ Key findings:
- For every 10% increase in porosity, the average fusion time is shortened by 3.2 weeks (p < 0.01)
- Through-hole structure reduces the risk of settlement by 87% (> 2mm is defined as failure)
4. Coordinated control of porosity and other parameters
Four-dimensional standard matrix of ASTM F3122-18:
- Structural dimension: porosity 60±5%, pore size 600±100μm
- Mechanical dimension: compression resistance>180MPa, shear resistance>90MPa
- Material dimension: Ti6Al4V ELI (ASTM F3001-14) or PEEK (F2026)
- Biological dimension: surface roughness Ra 20-50μm promotes cell attachment
How to Overcome Bioprinter Resolution Limitations for Capillary Networks?
1. Biological challenges of capillary networks
- Physiological scale limit: the diameter of the thinnest capillary is only 3-8μm (red blood cells need to deform to pass through)
- Structural complexity: the total length of human blood vessels is ≈100,000 kilometers, and the fractal branching reaches 12 levels
- Functional requirements: material exchange + hemodynamic simulation must be achieved
2. Technological breakthroughs: Three major innovations of XYZ nanoP 1200
Two-photon polymerization (2PP) super-resolution printing
- 2μm ultimate resolution (10 times higher than traditional extrusion printing)
- Non-contact photocuring: avoid mechanical stress damage to endothelial cells (survival rate > 98%)
Driven by biomimetic fractal algorithm
- 8-level branching structure (gradient change from 500μm to 8μm in diameter)
- Spiral flow channel design: simulates the secondary flow effect of natural blood vessels (shear force fluctuation < 5%)
Living cell-friendly materials
- Gelatin-alginate composite hydrogel (elastic modulus 1-5kPa adjustable)
- RGD peptide modification: promotes directional arrangement of endothelial cells (adhesion density increased by 3 times)
3. Myocardial tissue engineering results of Harvard Medical School
| Parameters | Vascular network group | Vascular-free group |
|---|---|---|
| Survival period | >6个月 | Necrosis in 3 weeks |
| Contractile force | 12kPa | 4kPa |
| Drug test consistency | 92% vs human data | only 47% |
▶ Key mechanism:
Printed vascular network perfusion speed 15mL/min (meet myocardial oxygen demand)
Endothelial cells form tight junctions (TEER value >200Ω·cm²)
4. Comparison with mainstream technologies: the balance between resolution and throughput
| Technology | Resolution | Maximum throughput | Vascular grading capability |
|---|---|---|---|
| Two-photon polymerization | 2μm | 1mm³/h | Level 8 |
| Micro extrusion | 50μm | 50mm³/h | Level 3 |
| DLP photocuring | 25μm | 20mm³/h | Level 4 |
| Suspension printing | 10μm | 5mm³/h | Level 6 |
5. Clinical transformation path: from organ chips to transplantation
- Short term (2025): Liver lobule chips (including bile duct network) for drug hepatotoxicity testing
- Medium term (2030): Microvascular patch transplantation for diabetic foot ulcers
- Long term (2035): Construction of vascular tree framework for whole-organ printing
What Cybersecurity Standards Apply to Medical 3D Printing Systems?
1. Why does medical 3D printing require special cybersecurity standards?
- Data sensitivity: 1 patient image data contains 50,000+ anatomical feature points (reconstructable facial recognition)
- Device networking risk: 90% of medical 3D printers have unencrypted G-code transmission vulnerabilities (FDA warning)
- Strictness of regulations: Data breaches can be fined up to 4% of a medical institution’s annual income (GDPR regulations)
2. 7 core standard systems (comparison between China, the United States and Europe)
| Standard category | International standard | China requirements | Key control points |
|---|---|---|---|
| Image data transmission | DICOM PS3.15 | YY/T 1709-2020 | Mandatory compliance with IEC 62443-3-3 industrial security |
| Data encryption | HIPAA §164.312 | CFDA”Guidelines for Medical Data Security” | AES-256+blockchain double insurance |
| Equipment security | FDA 21 CFR 820 | GB/T 25070-2019 | Print instruction signature (RSA-3078) |
| Access control | ISO/IEC 27001 | Information Security Protection Level 2.0 | Retina + voiceprint biometrics |
| Log audit | NIST SP 800-92 | JR/T 0071-2020 | Blockchain evidence storage (10ns timestamp) |
| Emergency response | HITRUST CSF | National Health Commission emergency plan | AI threat perception (301 Hospital intercepted 12,700 times) |
| Supply chain security | NIST SP 800-161 | Medical Device UDI Traceability | 3D Printing Material Batch Blockchain Registration |
3. Data security protection system of neurosurgery of 301 hospitals (2023 annual operation data)
DICOM image transmission security
- Deploy an industrial-grade firewall system that complies with the IEC 62443-3-3 international standard
- Carry out the testing and verification of quantum key distribution (QKD) technology to prevent the risk of quantum computing attacks in the future
Patient medical data encryption protection
- The AES-256 encryption algorithm is used to protect the original CT data, and the theoretical cracking time is more than 1.5×10⁵³ years
- Based on Hyperledger Fabric blockchain technology, the operation log cannot be tampered with
System protection effectiveness statistics
- Successfully intercepted 12,700 illegal access attempts throughout the year, with a 100% interception success rate
- The medical data desensitization processing capacity reaches 5,000 cases/hour, and the anatomical features required for clinical use are completely preserved
Explanation of international standard compliance differences
Key differences:
- China’s CFDA specifically requires the use of blockchain evidence preservation technology
- The US FDA is certified to accept the AES-128 encryption standard
- The EU GDPR requires data breaches to be reported within 72 hours
Conclusion
3D printing is reshaping the medical industry, with applications ranging from device manufacturing to biotissue engineering. With the advantages of personalized customization and precise matching, it has greatly improved the treatment effect and has been widely used in orthopedic implants, prosthodontics and surgical guides. For example, 3D printing can customize orthopedic implants according to the patient’s bone structure and condition, improving the success rate and postoperative comfort. The oral prosthesis is highly compatible with the patient’s oral cavity and has better aesthetics; The surgical guide provides doctors with precise operation guidance and reduces the risk of surgery.
In the future, with the innovation of bioprinting technology and smart materials, 3D printing is expected to make functional organs and alleviate the shortage of transplanted organs. The integration of 4D printing technology will give medical products the ability to self-adjust with time and environment, expanding the application boundary.
Despite the potential of 3D printing technology in the medical industry, it still faces challenges such as material safety and inadequate regulatory approval standards. However, there is no doubt that it has a bright future, and it is gradually reshaping the medical service model, and it is expected to become an important pillar of the future healthcare system.

📞 Phone: +86 185 6675 9667
📧 Email: info@longshengmfg.com
🌐 Website: https://www.longshengmfg.com/
Disclaimer
The content appearing on this webpage is for informational purposes only. LS makes no representation or warranty of any kind, be it expressed or implied, as to the accuracy, completeness, or validity of the information. Any performance parameters, geometric tolerances, specific design features, quality and types of materials, or processes should not be inferred to represent what will be delivered by third-party suppliers or manufacturers through LS’s network. Buyers seeking quotes for parts are responsible for defining the specific requirements for those parts. Please contact to our for more information.
Team LS
This article was written by various LS contributors. LS is a leading resource on manufacturing with CNC machining, sheet metal fabrication, 3D printing, injection molding,metal stamping and more.
FAQs
1.How is 3D printing used in healthcare?
3D printing is mainly used in healthcare to manufacture personalized medical implants (such as joint prostheses, skull restorations), surgical guides, dental restorations (crowns, dentures), bionic organ models (for preoperative planning), and customized drug preparations.
2.What is the future of 3D printing in healthcare?
In the future, 3D printing will focus on biological organ printing (such as heart and liver tissue), intelligent responsive implants (4D printing self-adjusting scaffolds) and personalized drug printing, combining AI-optimized design and bioactive materials to promote the development of regenerative medicine and precision medicine, and finally realize on-demand printing of transplantable organs with complete functions.
3.How is 3D modeling changing the medical field?
By converting medical images such as CT/MRI into 3D digital models, 3D modeling enables doctors to conduct virtual surgical drills, customize patient-matched implants, and improve the visualization of medical education, such as creating tumor vascular models to guide complex surgeries, or printing pathology specimens for teaching, improving the overall accuracy of diagnosis and treatment and the efficiency of education.
4.What are the common applications of 3D printing in the field of medical devices?
Key applications include: orthopedic implants (porous titanium interbody fusion devices), dental equipment (clear aligners, implants), surgical navigation tools (tumor resection guides), prosthetic orthoses and minimally invasive surgical instruments, such as hip prostheses manufactured with SLM technology to achieve more than 95% anatomical fit.


Pingback: What is HIPS 3D printer filament?